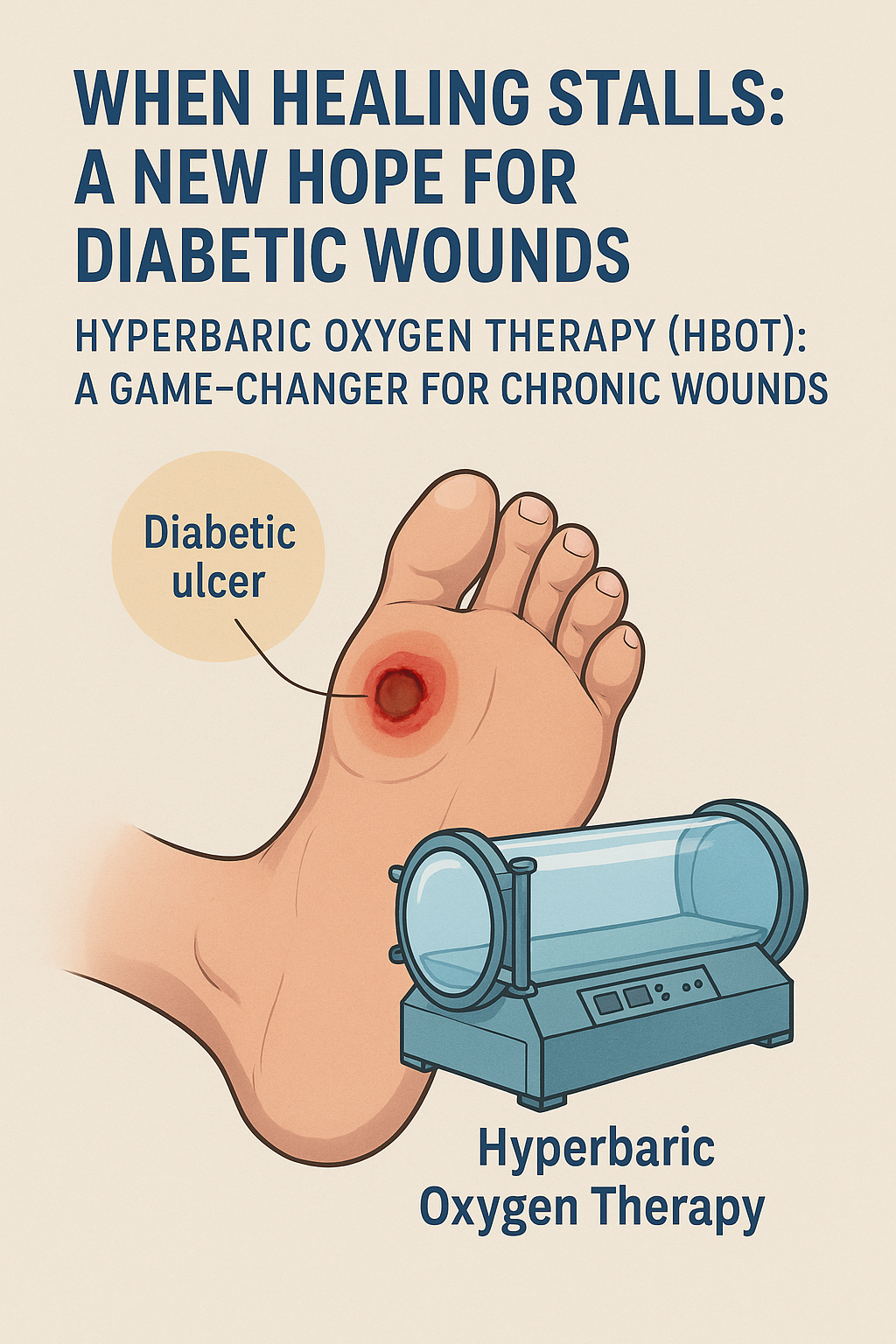
When Healing Stalls: A New Hope for Diabetic Wounds
Introduction
Diabetes is more than a blood sugar issue. For millions around the world, it silently erodes the body's ability to heal. Among its most insidious complications are chronic foot ulcers—wounds that refuse to close, becoming open doors to infection, amputation, and even death.The Hidden Crisis of Non-Healing Wounds
An estimated 15% of people with diabetes will develop a foot ulcer in their lifetime. These wounds, often small and painless in their early stages due to diabetic neuropathy, can quickly spiral into serious infections. What begins as a minor injury—perhaps from a poorly fitted shoe or unnoticed cut—can become a festering wound resistant to conventional treatments.Standard wound care protocols involve offloading pressure, debridement, infection control, and moist wound healing. Yet, even with meticulous care, many ulcers fail to respond. This is especially true in cases complicated by poor peripheral circulation or microvascular damage, which deprive the tissue of the oxygen and nutrients it desperately needs.The Cost of Failure
The human cost is staggering: diabetes is responsible for more than 80% of non-traumatic lower-limb amputations. But the financial burden is just as severe. Chronic wounds significantly increase hospital stays, outpatient visits, and long-term care. Worse still, patients who undergo major amputations have a 5-year mortality rate comparable to some cancers.Why Aren’t These Wounds Healing?
Wound healing is a highly orchestrated process involving inflammation, tissue regeneration, and remodeling. Oxygen is a critical player in every stage—from killing bacteria to forming new blood vessels. In diabetic individuals, however, this process is impaired. High blood sugar stiffens arteries, impairs immune responses, and restricts oxygen delivery—creating a biological “traffic jam” that blocks healing at every turn.So, What If We Could Deliver More Oxygen—Directly?
This is where a lesser-known but powerful therapy is making a difference.Hyperbaric Oxygen Therapy (HBOT): A Game-Changer for Chronic Wounds
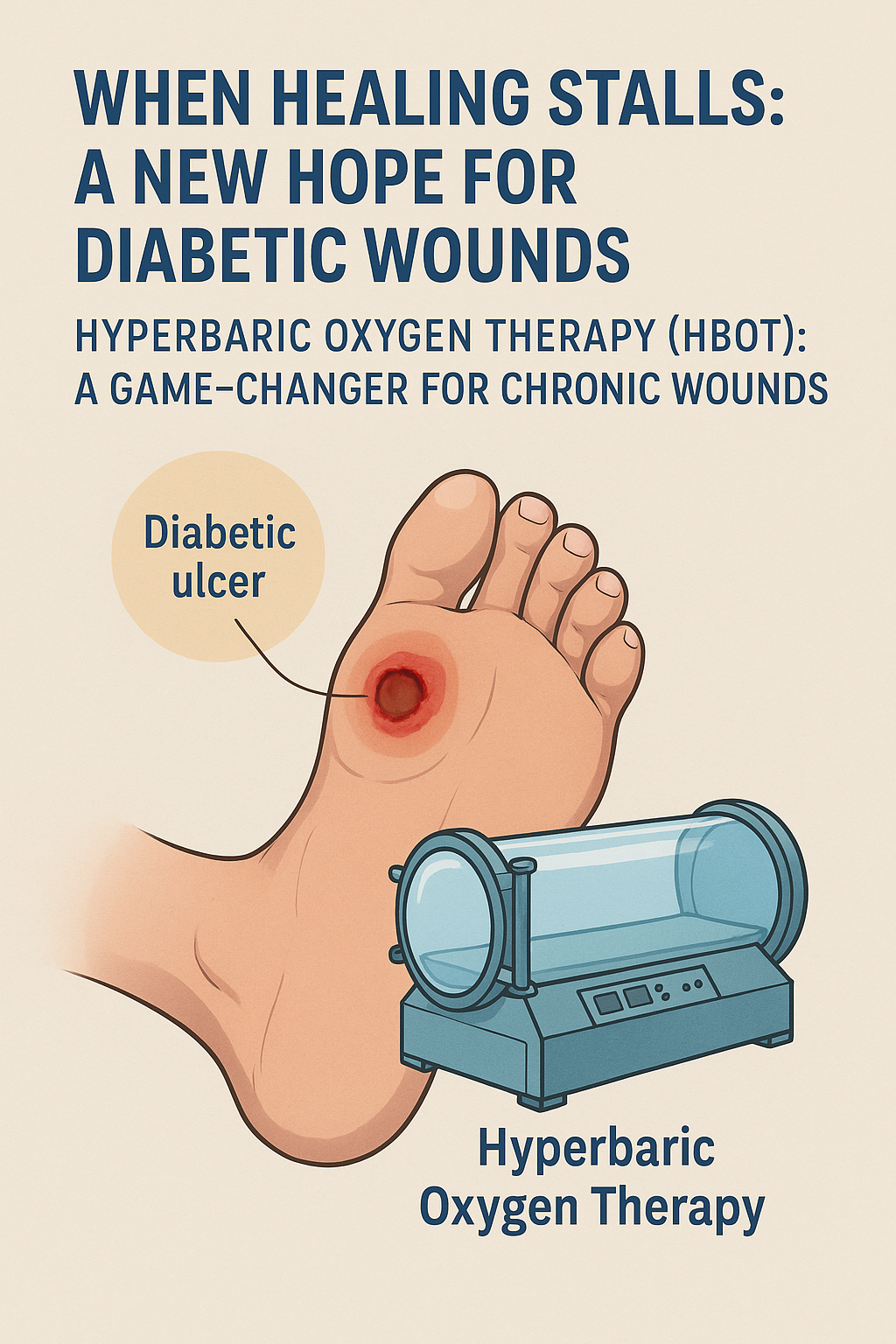
HBOT involves breathing 100% oxygen in a pressurized chamber, saturating the blood with oxygen and delivering it deep into tissues that have been starved of it. For diabetic wounds, this means:
- Enhanced collagen production and tissue repair
- Stimulated formation of new capillaries (angiogenesis)
- Boosted white blood cell activity to fight infection
- Reduction of inflammation and swelling
Clinical studies show that when used as an adjunct to standard care, HBOT significantly increases wound closure rates and reduces the need for amputations. It’s not a magic bullet—but in cases where healing has stalled, it can tip the balance.Conclusion: Healing Where Others Gave Up
For patients with chronic diabetic wounds, time is tissue. Each day that passes without healing increases the risk of devastating outcomes. In this high-stakes battle, oxygen itself becomes a medicine—and HBOT is the vehicle that delivers it.As healthcare continues to evolve, integrating advanced therapies like HBOT may redefine what’s possible in wound care—offering not just longer lives, but better ones.